SERVICES
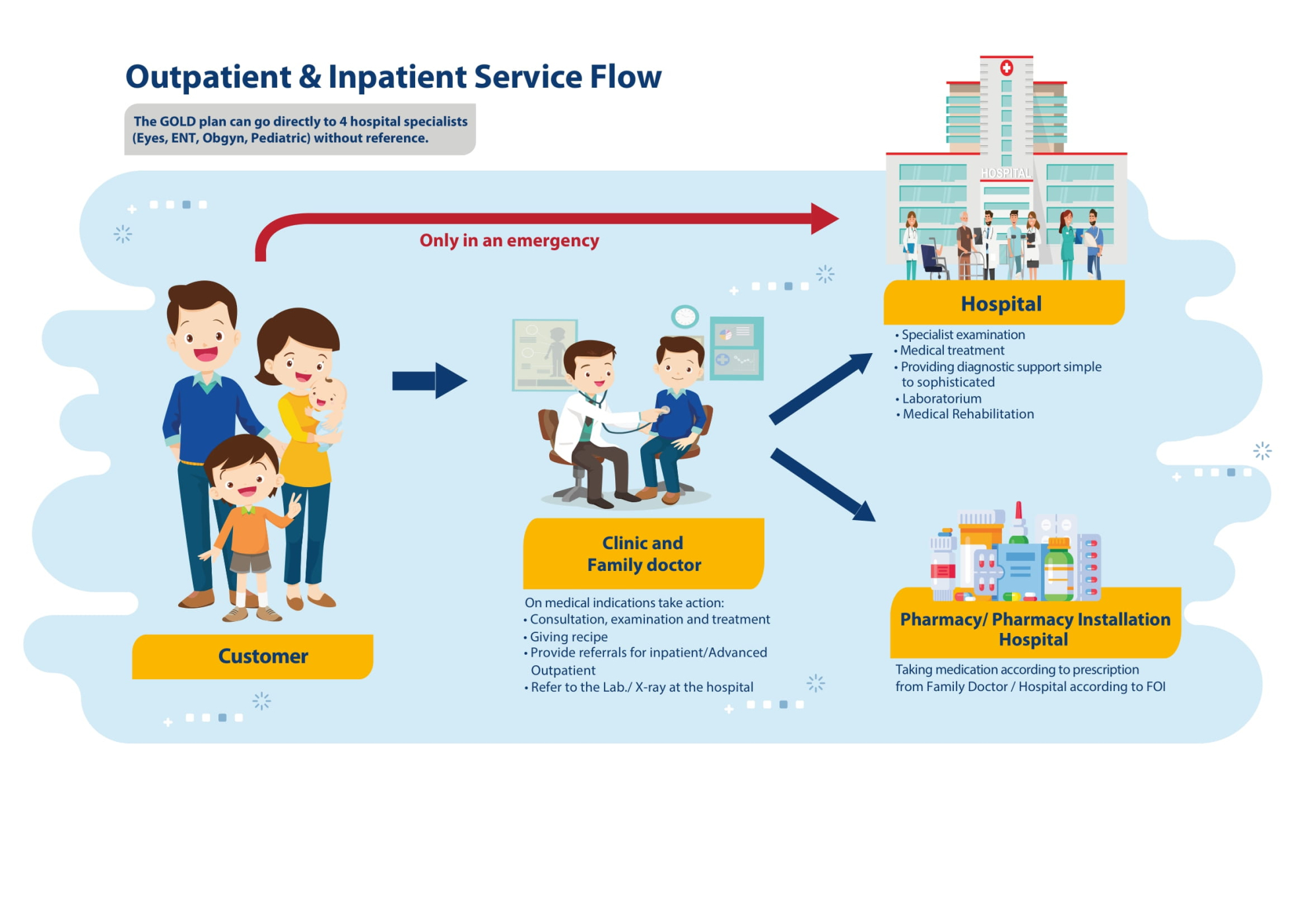
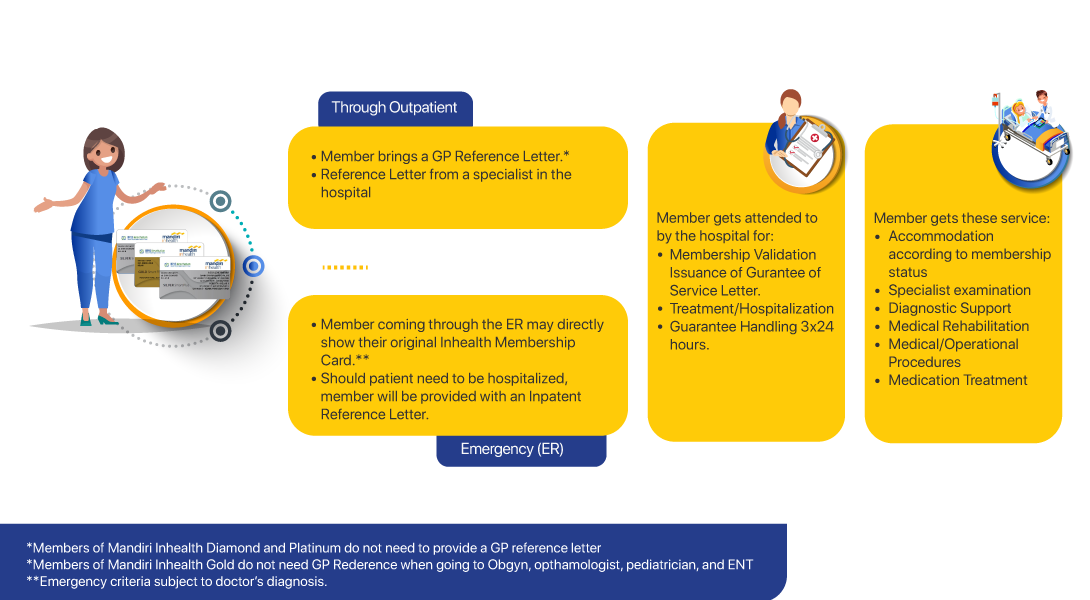
Services Mandiri InhealthProvider Managed Care
Managed Care is an efficient quality health insurance product in premium financing. Here, the insurance company works with health care providers (hospitals, clinics, laboratories, etc.) to provide cost-effective services to participants.
This is an application that serves to know all the information about the Provider (hospital, family doctor / clinic, pharmacy, laboratory, optics) and Provider Relation Officer (PRO) Mandiri Inhealth.
Provider Indemnity
Information about Providers (hospitals, clinics, pharmacies & dentists) partnered with Mandiri Inhealth.
Click the link below to find out the Provider / Health Insurance Service List of Inhealth Indemnity:
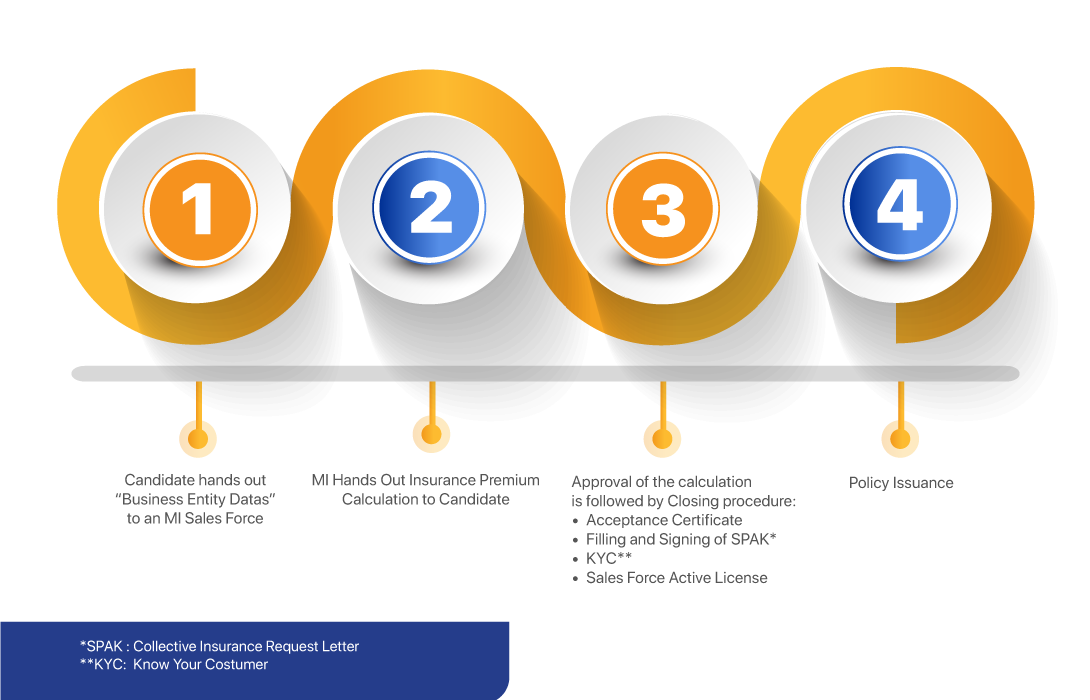
Procedure for transacting
Get information on how to partnering with Mandiri Inhealth
FitAja!
FitAja merupakan aplikasi kesehatan digital yang dikembangkan untuk memenuhi berbagai macam kebutuhan layanan kesehatan mulai dari layanan preventif hingga rehabilitatif di dalam satu aplikasi.
Layanan yang ditawarkan yaitu, akses info peserta (FitMe), konsultasi online dengan dokter melalui chat, telepon, ataupun Video Call (FitTele), info daftar obat FOI (FitMedicine), info benefit asuransi (FitBenefit), mencari provider terdekat (FitProvider), pengajuan klaim online (FitClaim), pendaftaran Faskes melalui QR code (Fitcode), serta beberapa layanan lainnya yang masih dalam tahap pengembangan.

Mandiri Inhealth activities
Testimoni Peserta Prioritas Mandiri Inhealth
Alur Pelayanan Klaim Peserta Mandiri Inhealth dan Testimoni
HealTea Talk Eps.2 - Sakit Jantung / Kardiovaskular: Penyebab Kematian Terbesar di Dunia
Formularium Obat Inhealth (FOI)
Counter & Lounge Khusus Peserta Mandiri Inhealth
HealthTea Talk - Mitos & Fakta Penyakit Asam Urat
Testimoni Mandiri Inhealth Contact Center
Testimoni Peserta Prioritas Mandiri Inhealth
Media

Inhealth Gazette
October 2023 edition
Inhealth Gazette
August 2023 Edition
Inhealth Gazette
Juli 2023 Edition
Inhealth Gazette
2023 June Edition
Inhealth Gazette
May 2023 Edition
Inhealth Gazette
April 2023 Edition
Inhealth Gazette
March 2023 Edition
Inhealth Gazette
February 2023 Edition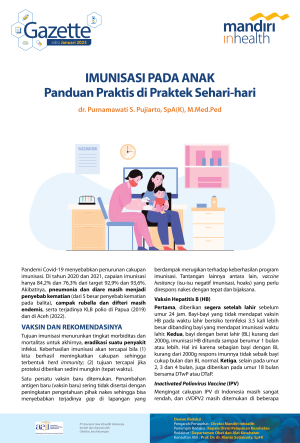
Inhealth Gazette
January 2023 edition
Inhealth Gazette
November 2022 Edition
Inhealth Gazette
October 2022 Edition
Inhealth Gazette
September 2022 edition
Inhealth Gazette
July 2022 Edition
Inhealth Gazette
June 2022 edition
Inhealth Gazette
March 2022 edition
Inhealth Gazette
February 2022 edition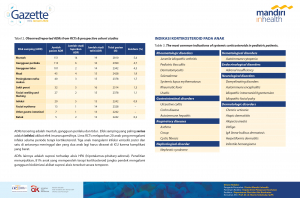
Inhealth Gazette
January 2022 edition
Inhealth Gazette
November 2021 Edition
Inhealth Gazette
December 2021 Edition
Inhealth Gazette
October 2021 Edition
Inhealth Gazette
September 2021 Edition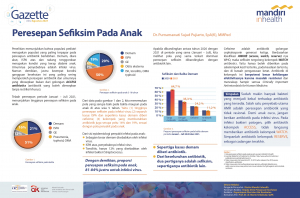
Inhealth Gazette
August 2021 edition
Inhealth Gazette
2018 Edition
Inhealth Gazette
2018 Edition
Inhealth Gazette
2017 Edition
Inhealth Gazette
2016 Edition
Inhealth Gazette
2015 Edition
Inhealth Gazette
2014 Edition
The Importance of Balance between Diet and Physical Activity
April - June 2024 Edition
Importance of Physical - Mental Wellbeing
January - March 2024 Edition
Skin Cancer and Symptoms
October-December 2023 Edition
Influenza and the Use of Telemedicine Apps
July-September 2023 issue
Reproduction System
April - June 2023 issue
Recognise Measles Symptoms Early
January - March 2023 Edition
Kidney Disease in Children
October - December 2022 issue
Transition season
Edition July - September 2022
650 CASES OF ACUTE HEPATITIS DISCOVERED SINCE APRIL INDONESIA IS MORE ALERT!
April - June 2022 edition
Beware of Silent Killer Kidney Disease Symptoms
January - March 2022 edition
Make a Resolution in 2022
Edition October - December 2021
Mental Health: Between Awareness and Stigma Public
July - September 2021 Edition
Spinal Disorders
April - June 2021 edition
Peel Thoroughly Regarding Covid Vaccination 19
January - March 2021 Edition
Peel Thoroughly Obesity Problem
October - December 2020 Edition
Personal Hygiene, Key to Early Healthy Life
July - September 2020 Edition
Stay Healthy and Productive Work
April - June 2020 edition
Know more about rheumatism
Januari - Maret 2020 Edition
Mandiri Inhealth Health the Country
October - December 2019 edition
Customer Day 2019 mi-health, inspiration for those you love
Juli - September 2019 Edition
How Hating your Job Affects Your Body
April - Juni 2019 Edition
Importance of Nutrition Consumption for the Body
Januari - March 2019 Edition
Celebrating 10 Years of Mandiri Inhealth
Oktober - Desember 2018 Edition
Stop Hepatitis
Juli - September 2018 Edition
Specter for Mother's Pregnancy
April - June 2018 Edition
Don't Think Underestimate Throat Inflammation
January - March 2018
One Spirit, Healthy My Country
Oktober - December 2017 Edition
Keep Your Eye Health in the World
July - September 2017 Edition
Alert! Aloe Cancer Similar Thrush
January - March 2017 Edition
Fasting, how come weight gain actually increases
April - June 2017 Edition